With ME/CFS* or Long COVID, your old life fades away. You lose contact with family and friends. You have to explain your illness again and again. Even your doctor doesn’t understand what is happening to you.
You are not alone. A staggering 85 million individuals face multisystem diseases like ME/CFS and Long COVID.
*ME/CFS is also known as myalgic encephalomyelitis and chronic fatigue syndrome.

ME/CFS and Long COVID disrupt many body systems. Traditional research looks at one system at a time. That approach doesn’t work.
That’s where Open Medicine Foundation (OMF) comes in. As a nonprofit, we’ve raised more than $50 million to fund open collaborative research. OMF brings world-renowned scientists together to study, diagnose, treat, and cure complex diseases.
It’s a bold dream. It’s the path that will get you back to a fulfilling life.
Once we understand how ME/CFS and Long COVID develop, researchers can pinpoint targets for intervention.
ME/CFS and Long COVID are difficult conditions to diagnose. We need specific biomarkers and definitive tests.
Currently, there are very few treatments and they only target symptoms. OMF launched its first treatment trial in 2023.
OMF provides medical education to help healthcare providers understand the challenges of multisystem disease.

6 Neuroendocrine Studies
"Neuroendocrine" refers to the interactions between the nervous system which controls
body functions through nerve impulses, and
the endocrine system which regulates body
functions through hormones.
3 Immune Studies
The immune system defends the body against infections and diseases, helping to maintain overall health.
3 Cardiovascular Studies
The cardiovascular system, comprising the heart, blood vessels, and blood, is responsible for transporting oxygen, nutrients, hormones, and waste products throughout the body.
10 Metabolism Studies
Multiomics is a scientific approach that can include genomics, proteomics, metabolomics, and transcriptomics to get a comprehensive understanding of biological systems. Abnormalities in carbohydrate, lipid, and amino acid metabolism have been observed.
1 Genetics Study
Genetics may contribute to an individual's susceptibility to multisystem disease, including variations in immune system genes, genes involved in energy metabolism, and genes related to neurotransmitter function.
12 Multi Omics Studies
Multiomics combines various omics technologies such as genomics, transcriptomics, and proteomics.
11 Diagnostic Studies
Diagnostic studies will help identify specific biomarkers towards differentiating between ME/CFS and illnesses with similar clinical presentations.
2 Treatment Studies
Treatment studies evaluate the efficacy and safety of potential interventions. Focusing on repurposed drugs could quickly provide evidence-based guidelines for healthcare providers.
4 Systems Biology Studies
Systems biology is an interdisciplinary approach that can help identify key pathways, biomarkers, and potential therapeutic targets.
4 Pathogen Studies
Infections can trigger or worsen a wide range of symptoms.
By funding studies that examine multiple systems, researchers can see how ME/CFS and Long COVID develop. This approach will lead to more effective treatments and improved quality of life.
Click on each system to read a description.







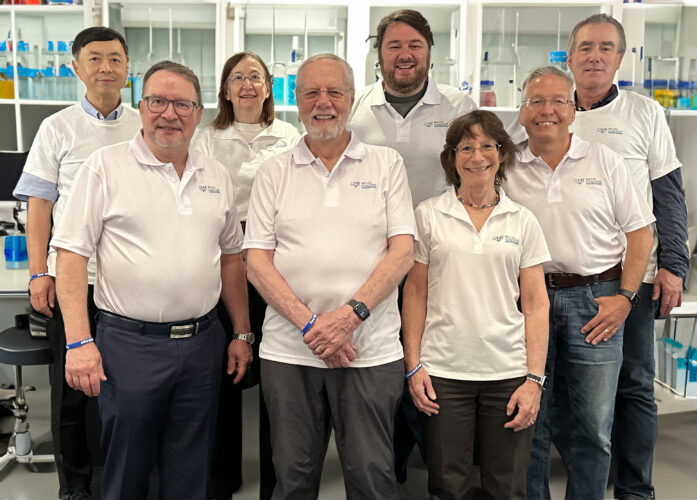
We get it. We, too, are patients, parents, or partners of someone with multisystem disease. We are passionate about finding a cure.
At OMF, research is a team sport. We take a systems biology approach at our seven global Collaborative Research Centers. We have a world-renowned Scientific Advisory Board overseeing the process. Instead of waiting on publications, we share results in real-time.
OMF believes multisystem disease should not be a life sentence but a solvable puzzle.





What will happen if research remains focused on one system at a time?
How will your life shrink? How many graduations, birthday parties, or everyday activities will you miss? What will happen with your career?
Something has to change.

OMF partners with leading research institutions worldwide.
OMF brings together brilliant scientists from around the globe.
Open collaborative research will unlock the door to treatments and cures. With your help, we can get to life-changing answers faster.
With your support, OMF funds groundbreaking research and medical education. We bring hope to those who need it most.
We bring together top researchers in multiple specialties — scientists dedicated to diagnosing, treating, and ultimately curing ME/CFS and Long COVID. They share data, collaborate, and build on each other’s work.
Even small breakthroughs can make a big difference when scientists share their ideas.
Unlike traditional research, we don’t wait for publication before we communicate our findings. We regularly post research updates on our website and through email. Make sure you subscribe to our latest news.

Perfect for printing and sharing with your doctor or personal community.
Open Medicine Foundation (OMF) is a US based global nonprofit, with an affiliate organization in Canada (OMF Canada) and a foreign branch in Australia (OMF Australia).
OMF is a non-profit 501(c)(3) organization
(EIN# 26-4712664). All donations are tax-deductible to the extent allowed by law.



Open Medicine Foundation®
29302 Laro Drive, Agoura Hills, CA 91301 USA
Phone: 650-242-8669
info@omf.ngo
Copyright © 2023 Open Medicine Foundation. All Rights Reserved.
Get the latest updates delivered to your inbox.
What are the advantages of giving from your Donor Advised Fund (DAF)?
How do I make a donation through my DAF?
Just click on the DAF widget below. It is simple and convenient to find your fund among the over 900 funds in our system.
Still can’t find your fund?
Gifting of Stock
Broker: Schwab
DTC #: 0164
Account #: 47083887
Account Registered as:
Open Medicine Foundation
29302 Laro Drive
Agoura Hills, CA 91301
Please speak to your personal tax advisor and then email or call OMF at 650-242-8669 to notify us of your donation or with any questions.